1DMD, Clinical Assistant Professor, New York University College of Dentistry
2DDS
The goal of this article focuses on how to restore patients who have severe loss of function and aesthetics. The patient, a 55-year-old male, presents with the chief complaint: “I came to get looked at and see what could be done for my teeth”. The patient initially presents with multiple broken and missing teeth (Figure 1). Past medical history is positive for seasonal allergies, Crohn’s disease, high cholesterol, osteoporosis, and thyroid disorder. The patient has no known drug allergies and has been taking aspirin (81 mg) for fi ve years as ordered by his primary physician. The extra-oral exam reveals an altered facial profi le. The lips appear thin and fl attened as if crunched. The chin has moved forward and upward. The mouth has lost shape and the lip lines have a reverse smile line. During the temporomandibular joint (TMJ) exam, the joints are load-tested. The centric relation position is considered obtained when the TMJ could be guided bimanually (with no sign of tension or pain) while the condyles were in their most superior anterior position within the glenoid fossa1,2. The TMJ is tested via careful palpation and transposition of its components to identify painful loci within the opening and closing of the arches. After manipulating the mandible into centric relation, it is realized that the patient has suffi cient interarch space to restore the patient to comfortable vertical dimension of occlusion.


Centric relation is needed to be verifi ed because it is the reproducible position utilized to restore a functional dentition3.Three main factors must be analyzed to establish a proper occlusal vertical dimension, according to Vierheller. These are: 1) the rest position, 2) the free-way space (interocclsual distance), 3) the vertical dimension of occlusion4. The vertical dimension at rest is analyzed using the act of swallowing as a guide to the physiologic rest position of the mandible5. The intraoral exam reveals an anterior impinging bite with teeth #8, 9, 10 and the mesial of tooth 11 contacting the mandibular anterior alveolar ridge. Clinical examination reveals missing maxillary teeth #5, 6, 7, 12, 13 (Figure 2) and mandibular teeth #17, 18, 19, 20, 23, 24, 25, 26, 29, 30, 31, and 32. Teeth #11 and 22 exhibit severe wear facets into pulpal chambers, but contact each other at an edge-to-edge position (Figure 3).


When guided into a functional centric relationship as defi ned by Dawson, the mesial marginal ridges of tooth #4 makes contact with the distal aspect of tooth #28 (Figure 4). The mandibular alveolar ridges are atrophic bilaterally (Figure 5). Both radiographic and clinical examination of the remaining teeth show advanced periodontal disease. There are many dental issues that must be addressed for this case. Certain posterior teeth with defective marginal seal of old amalgam restorations must be replaced. The remaining anterior teeth have wear facets associated with the collapsed vertical dimension of occlusion because of the lack of bilateral mandibular posterior occlusion. As a result, the maxillary dentitions have begun to drift vertically (supraerupted). There are two root tips with radiographic apical pathology compounded with gingival inflammation. The mandibular anterior gingiva is traumatized particularly in the anterior due to the severe abrasion of the lower incisors to the gingival level. Once medical and dental history examinations are evaluated, three sets of alginate impressions are made: 1) existing master casts, 2) diagnostic wax-up casts, 3) working casts. On the following visit, maxillary records are obtained via a Hanau facebow registration (Whip Mix Corp., Louisville, KY, U.S.A.). Two marks are placed on the patient’s face. The first mark is located above the upper lip and the second one is marked below the lower lip (Figure 6).

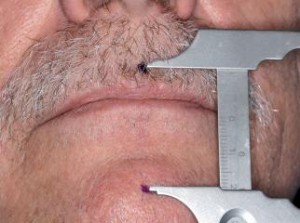
The rest position is recorded by measuring the patient’s vertical dimension between two points after the act of swallowing. The vertical dimension of rest is established at this point after consistency is achieved and the dimension is recorded using a Boley gauge caliper (Rudolf Manz GmbH & Co. KG, Germany). The height of both maxillary and mandibular occlusal wax rims are adjusted until the same vertical dimension of rest is established. Then the mandibular occlusal wax rim is reduced by 3 mm to establish a tentative occlusal vertical dimension. A study by Ward and Osterholtz presents an average of 2.78 mm of interocclusal distance using an indirect technique and an average of 3.5 mm using
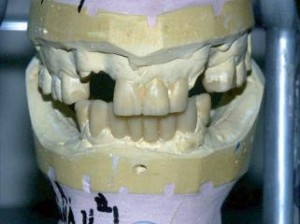
a direct technique. A fabricated Triad occlusal wax rim (Dentsply Prosthetics, York, PA, U.S.A.) is utilized with GC pattern resin (GC America Inc., Alsip, IL, U.S.A.) for a centric relation record. This centric relation record will be used to restore the vertical dimension of occlusion. The maxillary cast is then mounted using a Hanau semi-adjustable articulator (Whipmix Corp., Louisville, KY, U.S.A.), and sent to a dental laboratory with a prescription authorization for a wax-up of the anterior teeth that are broken or missing (Figure 7) and of the posterior teeth setup at the “restored” vertical dimension of occlusion. These diagnostic aides are used to formulate treatment plans to be presented to the patient.